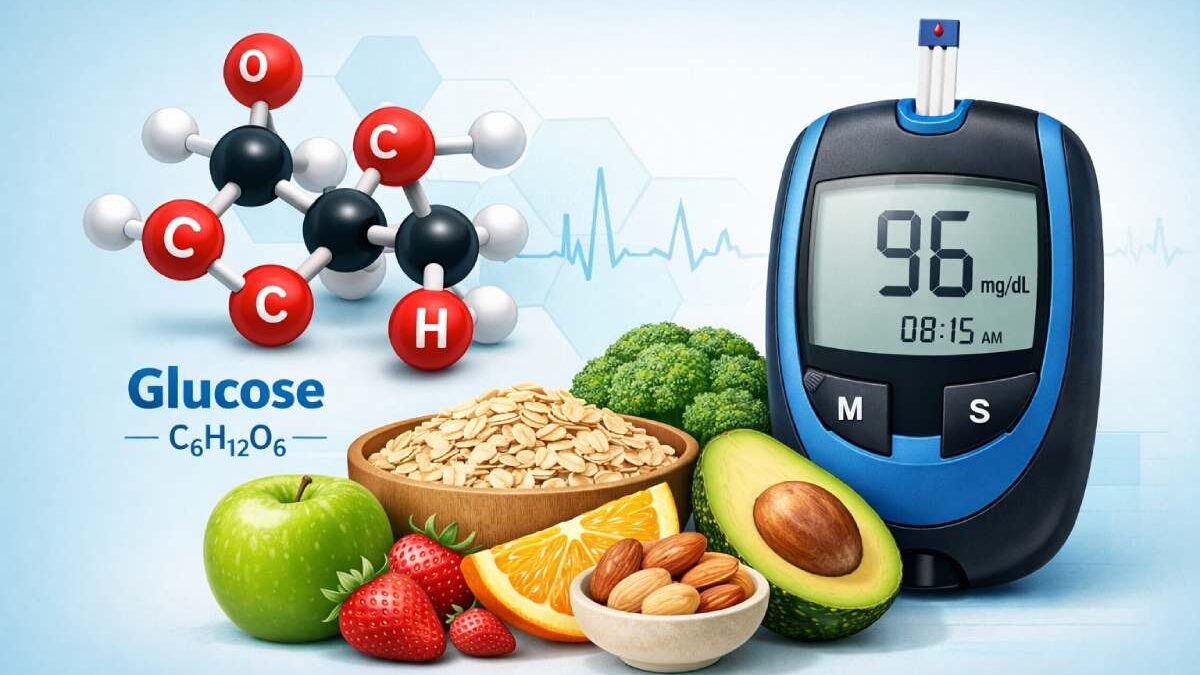
Glucose is a simple sugar (monosaccharide) that is the primary source of energy for cells in humans and most other organisms. It circulates in the blood and is tightly regulated by hormones — mainly insulin and glucagon.
Glucose fuels everything from brain function to muscle contraction. When blood glucose is too high or too low, it signals a metabolic imbalance that may need medical attention. This article covers what glucose is, how the body handles it, normal and abnormal blood levels, the tests clinicians use, real-world tips, and recent updates (including continuous glucose monitoring advances).
Table of Contents
American Diabetes: Why readers search “What is glucose?”
People usually want to know:
- What glucose actually is (simple definition).
- Which blood sugar levels are normal vs. abnormal.
- How glucose is tested and interpreted (FPG, OGTT, A1c, CGM).
- What steps to take if results are abnormal (prevention, treatment).
This article answers all of those clearly and with current references.
How the body processes glucose
- Intake & digestion: Carbohydrates from food are broken down into glucose in the gut.
- Absorption: Glucose enters the bloodstream from the intestine; blood glucose rises after meals (postprandial).
- Insulin release: The pancreas detects higher blood glucose and releases insulin. Insulin helps cells (muscle, fat, liver) take up glucose and lowers blood glucose.
- Storage & use: Excess glucose is stored as glycogen in liver and muscle; when needed, glucagon and other signals release glucose back into the blood.
- Energy generation: Inside cells, glucose is used in glycolysis and the Krebs cycle to produce ATP (cellular energy).
This tight hormonal control keeps blood glucose in a narrow optimal range. When these systems fail — for example when the body does not produce enough insulin or becomes insulin resistant — chronic hyperglycemia (diabetes) can occur.
Normal blood glucose levels – practical numbers
Below are standard reference ranges used in clinical practice for nonpregnant adults:
- Normal fasting plasma glucose (FPG): 70–99 mg/dL (3.9–5.5 mmol/L).
- Impaired fasting (prediabetes): 100–125 mg/dL (5.6–6.9 mmol/L).
- Diabetes (diagnostic fasting): ≥126 mg/dL on two separate occasions.
- 2-hour OGTT (75 g) normal: <140 mg/dL (7.8 mmol/L); impaired glucose tolerance: 140–199 mg/dL; diabetes: ≥200 mg/dL.
- HbA1c (glycated hemoglobin): Normal < 5.7%; prediabetes 5.7–6.4%; diabetes ≥6.5%.
Note: Reference ranges and diagnostic cutoffs are standardized by bodies such as the American Diabetes Association and WHO; small lab-to-lab differences exist, and clinicians interpret results in context.
Diagnostic tests – what they are and when they’re used
1) Fasting Plasma Glucose (FPG)
- What: Blood draw after an 8-hour fast.
- When used: Screening, routine checks.
- Cutoffs: See ranges above.
- Pros / Cons: Simple and widely available; can miss post-meal abnormalities.
2) Oral Glucose Tolerance Test (OGTT)
- What: Fast, drink a 75-g glucose solution; blood measured fasting and at 2 hours (sometimes 1 hour).
- When used: Suspected impaired glucose tolerance, pregnancy (gestational diabetes uses a modified protocol), or unclear FPG/A1c.
- Important notes: The 2-hour post-load value is a sensitive indicator of how the body handles glucose; the test must be performed under standardized conditions (morning, rest before test).
3) Hemoglobin A1c (HbA1c)
- What: Measures average blood glucose over ~3 months by glycation of hemoglobin.
- When used: Screening and monitoring long-term control.
- Limitations: Less accurate with hemoglobinopathies, recent blood loss/transfusion, or some anemias. Clinicians consider context and may use FPG/OGTT when A1c is unreliable.
4) Random (Casual) Plasma Glucose
- What: Any time of day without fasting.
- Diabetes threshold: ≥200 mg/dL with classic symptoms of hyperglycemia.
- Use: Rapid assessment in symptomatic patients.
5) Continuous Glucose Monitoring (CGM)
- What: Small sensor under/near the skin measures interstitial glucose every few minutes and transmits data to a receiver/app.
- Use: Day-to-day glucose patterns, time in range (TIR), hypoglycemia detection. CGM is standard of care for many people with type 1 diabetes and increasingly used in type 2 diabetes management. Recent FDA approvals (e.g., implantable Eversense 365) and evolving guidelines expand CGM options. CGMs are also used for ambulatory glucose profiling and to prevent hypoglycemia with automated alerts.
Hypoglycemia and hyperglycemia — symptoms and action thresholds
Hypoglycemia (low glucose)
- Alert level: <70 mg/dL (<3.9 mmol/L) is considered low and warrants attention. Level 1 hypoglycemia: <70 and ≥54 mg/dL; Level 2 is <54 mg/dL (clinically significant). Treat promptly with fast-acting carbohydrate (15 g) and recheck in 15 minutes — the “15/15 rule.”
- Symptoms: Shakiness, sweating, confusion, blurred vision, palpitations, severe cases may cause seizure or loss of consciousness.
- When to call for help: If severe or if the person cannot safely swallow carbohydrates.
Hyperglycemia (high glucose)
- Concerning levels: Persistent fasting ≥126 mg/dL or 2-hour OGTT ≥200 mg/dL — diagnostic for diabetes; symptomatic random ≥200 mg/dL also concerning. Long-term hyperglycemia raises risk for cardiovascular disease, neuropathy, kidney disease, and retinopathy.
New & notable updates (2024–2026)
- CGM adoption is expanding: New devices (including longer-lasting implantables) and guidance for CGM use are broadening access and clinical indications; however, accuracy and regulatory oversight remain areas of clinician attention. Patients using CGMs still need confirmatory testing in some situations and education to interpret Time in Range (TIR) and trends.
- Diagnosis & A1c emphasis: Recent guidelines continue to support A1c as a diagnostic and monitoring tool but emphasize appropriate use (beware of limitations in certain populations). Clinicians use a combination of FPG, OGTT, and A1c for a reliable diagnosis.
How doctors interpret results — practical examples
- Example 1: FPG = 110 mg/dL, A1c = 5.8% → This fits prediabetes; clinician will recommend lifestyle measures (diet, activity, weight management) and periodic retesting.
- Example 2: FPG = 140 mg/dL on two occasions → Diagnostic for diabetes; further evaluation and individualized treatment plan (medication ± lifestyle) follow.
- Example 3: CGM shows frequent glucose <70 mg/dL at night → Investigate causes (medication timing/overdose, missed meals, insulin dosing) and adjust therapy; consider supervised care plan.
Practical tips for patients
- Don’t skip the fasting instruction before FPG or OGTT — results depend on it.
- Bring medication list to lab visits — some drugs affect glucose.
- Use CGM data wisely — discuss targets like Time in Range (TIR) with your clinician.
- Treat low glucose promptly with 15 g fast carbs (juice, glucose gel), then recheck after 15 minutes.
- Lifestyle works: Dietary changes, regular physical activity, and modest weight loss prevent or delay type 2 diabetes in many people with prediabetes. (See ADA lifestyle guidance.)
Common myths vs facts
| Myth | Fact |
| “If I have high glucose once, I have diabetes.” | One value is not diagnostic; repeat testing or use confirmatory tests (A1c/OGTT). |
| “CGM readings are 100% accurate.” | CGMs are very useful, but occasional discrepancies exist and clinical judgment is needed. |
| “A1c replaces all other tests.” | A1c is powerful but can be misleading in certain conditions (hemoglobinopathies, anemia); use combined testing when needed. |
When to see a doctor now
- Fasting glucose repeatedly ≥126 mg/dL or A1c ≥6.5%.
- Any random glucose ≥200 mg/dL with symptoms (thirst, polyuria, weight loss).
- Recurrent hypoglycemia (glucose <70 mg/dL).
- New symptoms of diabetes complications (vision changes, numbness, wounds that do not heal).
First-person expert note
In my clinical writing and patient education work, I’ve seen how simple tests like fasting glucose and A1c — paired with lifestyle coaching — prevent progression from prediabetes to diabetes for many people. I also regularly encourage patients who use CGM to meet with a diabetes educator for pattern analysis so device data becomes actionable rather than anxiety-provoking.
FAQs
Q: What is a normal fasting blood glucose?
A: Normal fasting blood glucose is usually 70–99 mg/dL (3.9–5.5 mmol/L).
Q: What tests diagnose diabetes?
A: Diabetes is diagnosed by FPG ≥126 mg/dL, 2-hour OGTT ≥200 mg/dL, or HbA1c ≥6.5% — usually confirmed by repeat testing.
Q: What is HbA1c?
A: HbA1c measures average blood glucose over ~3 months by examining glycation of hemoglobin; it’s used for both diagnosis and monitoring.
Q: How do I treat low blood sugar?
A: Use the 15/15 rule: take 15 grams of fast-acting carbs (juice, glucose tablets), wait 15 minutes, and recheck. Seek help if severe.
Q: Are CGMs safe and useful?
A: CGMs are valuable for trend data and hypoglycemia detection; newer devices (including implantable types) have extended wear and improved convenience, but device choice and interpretation should involve clinicians.
Final conclusion
What is glucose? — It’s the body’s primary energy sugar, tightly regulated to keep you healthy. Understanding glucose levels, how tests work, and what your results mean helps you take control of metabolic health. If a test shows abnormal glucose, follow up with your healthcare provider for personalized evaluation and a treatment plan that fits your health goals.